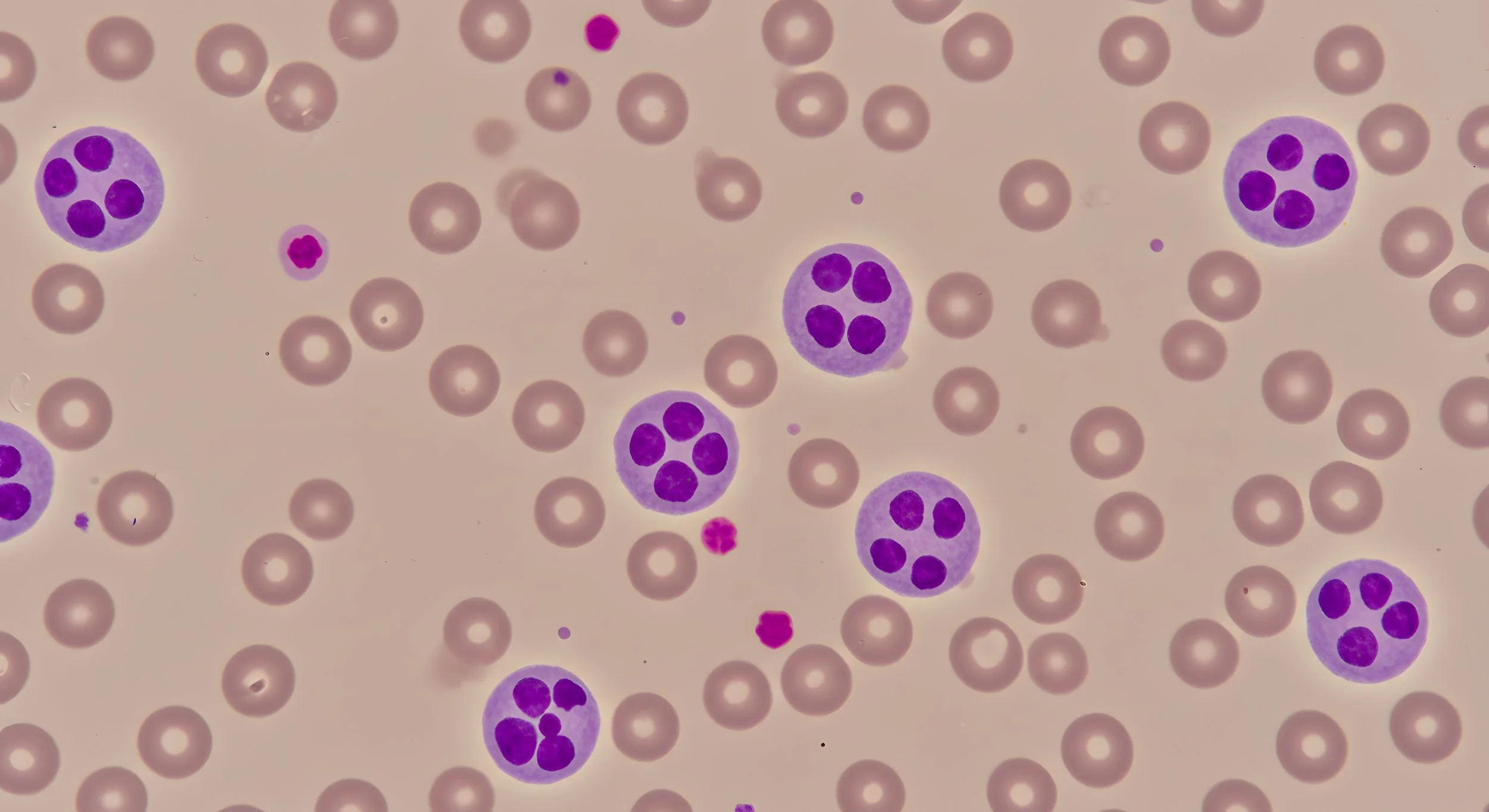
Meet Dr Lachie: Humanising Haematology and Making Medicine Understandable
Our resident Haematologist, Dr Lachie, has a passion for community care, clear communication, and making complex medicine less intimidating. From working across Melbourne’s north to helping set up pregnancy haematology clinics, Dr Lachie shares what drew him to the field, how medicine is changing, and why inclusive, flexible care matters now more than ever.
Hey Lachie! Thanks for taking some time to chat to me today. I’d love to start by asking - what inspired you to go into haematology?
I did a placement in endocrinology in Toronto and enjoyed it, but found it frustrating. When I came back to Melbourne, one of my first jobs was in haematology. It was tough - there weren’t many treatments for blood conditions back then, and a lot of very sick patients.
Over time, I tried a few different things, but haematology kept pulling me back. It was the most challenging, but I liked that. I also really enjoyed talking with people and helping them understand what was going on. Haematology has a lot of very complicated and evocative words. I liked breaking things down and using analogies to make it easier for my patients to understand what was happening to them. As treatments improved, the field got even more interesting and much more hopeful.
What kind of haematology do you specialise in?
I’m a general haematologist, which means I treat a bit of everything - anaemia, iron issues, blood clots, bleeding problems, and low-grade blood disorders. I also do a lot of work with pregnancy-related blood conditions, like iron deficiency or clotting issues.
I’ve always worked in the northern suburbs, mostly in clinics, helping people stay well and out of hospital. I’ve worked with lots of different communities and I try to make treatment plans that fit people’s needs - culturally, financially, practically. That includes things like finding medication alternatives if someone can’t take a certain medication due to religion, or using Google Translate to bridge language gaps. I try to keep things flexible for the patient.
What are some of the more complex parts of haematology that you help patients navigate?
There are a few!
Firstly, explaining things to patients. All the language in haematology is very complicated - breaking that down and telling people what it means is important. Related to that is fear, because haematology is rare - most people haven’t had a friend or relative who have had a blood disorder. There are certain words that are very evocative, such as the word ‘leukaemia’. I help to explain those terms in a way that is less confronting, and easier to understand.
Treatments for blood disorders can also be quite complicated and expensive. We used to just give chemotherapy to people with leukaemia which made people sick - now we also have other methods such as increasing immunotherapy, or combination therapy, or what we call small molecule therapy. This is good because people can increasingly choose to have their treatment in a day centre or take a tablet at home. Working out where is best for the patient (what treatments are available easily, what is affordable, what is culturally okay for them) is part of the complexity. Being a general haematologist, I need to be across all of that.
Dr Lachie is a general haematologist, which means he treats a bit of everything - anaemia, iron issues, blood clots, bleeding problems, and low-grade blood disorders.
You’ve done a lot in obstetric haematology — what’s that like?
I helped set up the pregnancy haematology clinic at the Northern. We treated things like anaemia, low platelets, and blood clots in pregnancy. Blood changes a lot during pregnancy, so we keep a close eye on things.
You’ve worked in the north for over 15 years — what’s changed?
So much! When I started, places like Craigieburn were half-empty. Now they’re booming. There’s been a big increase in young families and new migrant communities - Sikh, Syrian, Turkish, Macedonian - all looking for opportunities.
That’s brought a lot of diversity to the area, and a broader range of health needs. I’ve also noticed younger people expect a different kind of care - more agency, more flexibility. And I get it - things like the pandemic and housing crisis have made people more cautious about the system.
You live locally too — how does that shape your work?
I do! I live in Brunswick, so I’m part of the community. I shop local, I go to places like Compass Pizza and Toledo, and I see the same people out and about. It helps me stay grounded and understand what’s happening around me. I don't ride a bike though - I never got the confidence growing up in Adelaide!
What’s next for you?
A few things. I’d like to build a community-based haematology practice on the north side - something more accessible than the big hospital system. I’d also love to expand pregnancy haematology services at the Mercy and make them more sustainable and inclusive.
Long-term, I might not do clinical medicine forever. I’m interested in mentoring, especially for young people and those who are neurodivergent - coaching, support, helping people understand and navigate their health. That’s something I already do a lot of in practice, and I really enjoy it.
Who should come to see you?
Anyone with a general blood disorder - things like anaemia, clotting issues, or abnormal blood results. I don’t see kids under 16, but I do see a lot of women’s health and pregnancy-related blood issues. I’m also a big advocate for queer, trans, and neurodivergent folk to have safe spaces in healthcare. My practice is designed to be that. I have a trans daughter and a cis daughter, so this work is personal to me. Everyone deserves to feel respected and supported, and I want to help make that happen.
Book with Dr Lachie at Melbourne Specialty Centre today. Please note, you will need a GP referral.